Sometimes a scientific study can have a beneficial impact on the daily lives of many millions of people, as cardiologists Valentin Foster and Borja Ibáñez explain. A few months ago, his team presented the results of a clinical trial of 8,500 volunteers that showed that beta blockers—drugs that are prescribed for life after a heart attack for decades—“provide no benefit” to the majority of these patients, those who maintain their heart’s pumping ability. “We’ve been talking about millions of people in the world for decades, it’s barbaric,” Ibáñez sums up, in a room at the National Center for Cardiovascular Research (CNIC) overlooking northern Madrid. But his conclusions were met with some skepticism. A number of the Ministry of Health, family doctor Javier Padilla, left to declare that there were “contradictory articles in this area” and even criticized “Halazgos songs that can be very inflammatory.”
The controversy affects millions of people who spend a day or two with these tablets. Beta blockers can save your life if you have an irregular heartbeat, chronic heart failure, or heart dysfunction. These medications cause blood vessels to dilate, which reduces blood pressure and heart rate, but often has unwanted effects, such as persistent fatigue and decreased libido. You should only take it if there is a really medical reason. The Spanish team announces new results on Sunday, and this time they are “irrefutable,” according to Sopraya Ibanez, scientific director of the CNIC. The researchers analyzed data from five clinical trials in eight countries, involving 18,000 participants, and confirmed their previous conclusion: the ubiquitous beta-blockers are not necessary for patients who, after surviving a heart attack, maintain the correct contractile activity of their heart.
Ibanez tells the accounts. He estimates that in Spain alone there may be 1.2 million people taking beta blockers every day without needing them, but he claims that there are another 500,000 patients for whom only these medications are recommended. Nadia must abandon the treatment without consulting her cardiologist first, warning Ibanez and Foster. Its findings, which were presented on Sunday in Nueva Orleans (EE UU) at the Estadounidense del Corazón Association conference, were published in the specialized journal New England Journal of Medicine.
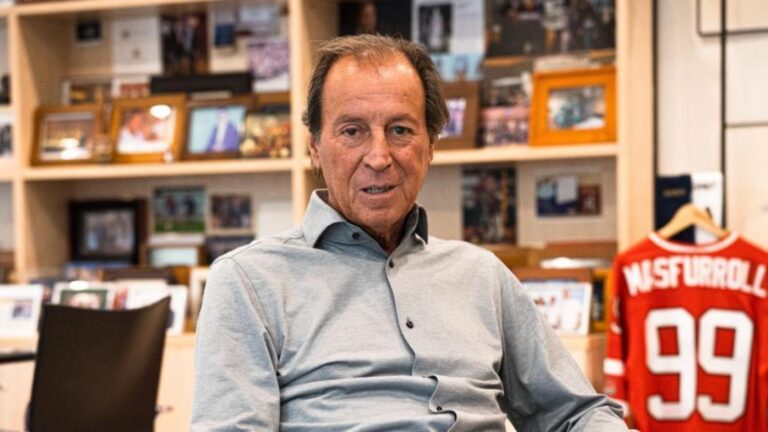
Valentin Fuster directs the CNIC in Madrid, and at the same time heads the Cardiaco Monte Sinaí Fuster Hospital in New York, which has borne his name for years. The famous cardiologist says he has been prescribing beta blockers to his patients suffering from complex heart attacks for a decade. He explains that it was not an easy decision. Foster is a student of Desmond Julian, the British doctor who conducted an ambitious clinical trial that demonstrated the benefits of beta blockers after a heart attack. However, the benefit of these drugs declined from 2005 onwards, when they were implemented Stents Coronary arteries, which are metal tubes that prevent blockage of the arteries, leading to a heart attack.
“I worked with Desmond Julian, where I lived the development of the beta-blocker concept for a long time. For a few years, it was like gospel: you had to give beta-blockers after a heart attack, just like that. I stopped giving them 10 years ago, but I was questioned a lot,” recalls Foster, who is born in Barcelona and is 82 years old. Your team is now working to calculate the savings generated by public health. Beta blockers are medications that date back to the 1970s and are off-patent, such as bisoprolol, developed by Merck Pharmaceuticals, and metoprolol, historically associated with AstraZeneca. A box containing 40 tablets costs four euros. It’s very cheap, but if 1 million patients stopped buying their daily capsule, the cost would be about 35 million euros a year, according to Ibanez’s first estimate. “We will save millions of people from public health,” he declared.
The new analysis includes nearly 18,000 volunteers, most of them from Spain, Sweden, Norway, Denmark, Italy and Japan. Everyone has had a heart attack, but without losing the heart’s ability to pump blood. Most patients received beta blockers and the other half did not. After four years of follow-up, doctors noted similar results in both groups: About 8% of participants experienced a major cardiovascular event, leading to heart failure, a new heart attack or even death. Take beta blockers or don’t change them at all. “This data is definitive,” Foster says.
His previous study, called REBOOT, which he conducted in one hundred hospitals in Spain and Italy, obtained alarming results among women. For every 100 patients treated with beta-blockers, there would be an outcome of death, re-infarction, or hospitalization due to the drugs themselves, the authors then explained. The publication of the Spanish-Italian research coincided with another similar study, but with a smaller number of patients, conducted in Denmark and Norway. The results seem contradictory. The Scandinavian work, which involved 5,600 volunteers, found that beta blockers slightly reduce the risk of death or serious cardiovascular disease. After analyzing all the data together, the hypothesized beneficial effect disappeared. The potential harmful effect on some women is now considered statistically significant.
In 2014, the European Society of Cardiology commissioned Borja Ibáñez to develop its guideline for the treatment of myocardial infarction, a problem that every year affects millions of people on the continent, 70,000 of them in Spain. The cardiologist reported that there is an absolute lack of evidence about the current effectiveness of beta blockers in uncomplicated heart attacks, despite the fact that millions of people take them daily. Thus, the idea of putting them to the test was born. “The result is revolutionary,” says Ibanez, who understands the skepticism of recent months. “Humans in general, and the medical community is no different, have a lot of fear of change, but among people who are experts in heart attacks, this data is not surprising to Nadi,” he says.
Ibanez and Foster expect that there will be an immediate change in guidelines for treating heart attacks around the world. Among the main authors of the new study are Danish cardiologist Eva Prescott, Japan’s Nico Ozasa, and Spain’s Xavier Rossello. The president of the Spanish Society of Cardiology, Ignacio Fernández Lozano, also believes that this international analysis casts doubts aside. He concludes: “Now 70% of patients remain without many complications or suffer a heart attack, while maintaining heart function, and they do not get the benefits of beta blockers, so there is no reason to give them.” This cardiologist, from Madrid’s Puerta de Hierro Majadahonda General Hospital, insists that no one stops their treatment without consulting their doctor first.