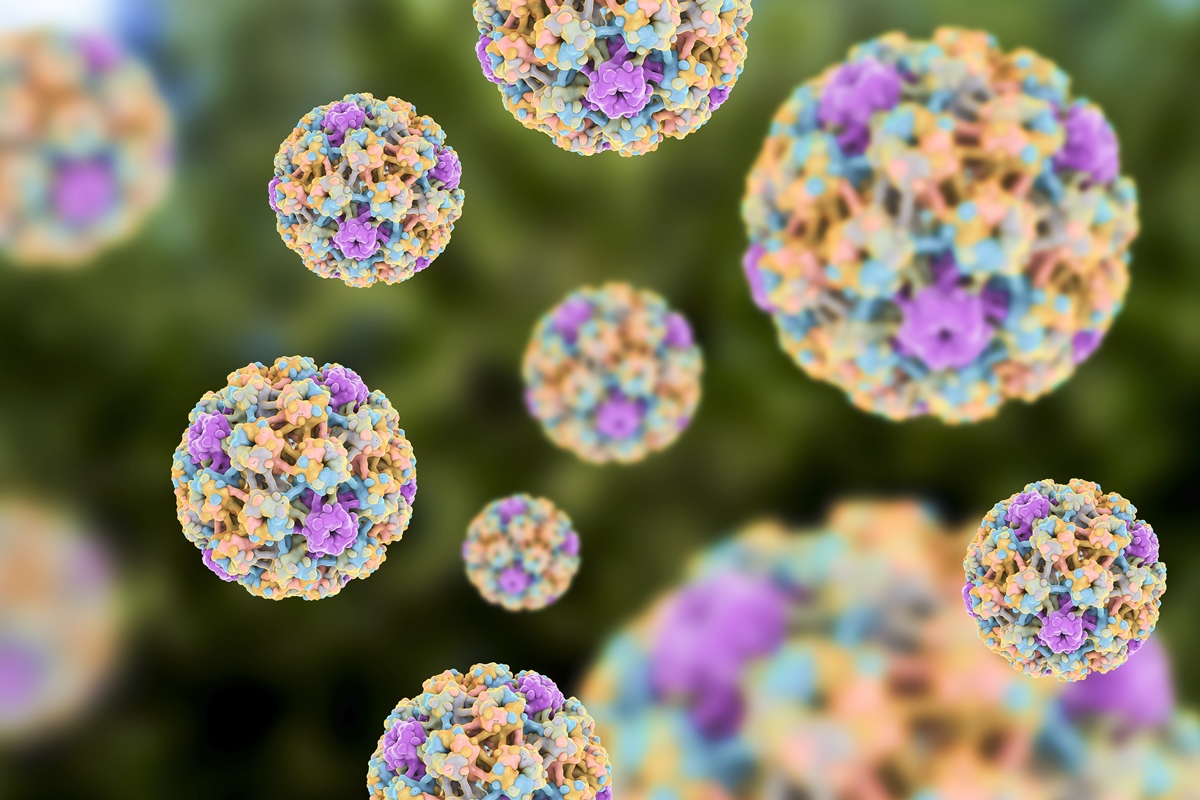
Thanks to advances in HPV vaccination, Brazil could be on the verge of eliminating one of the deadliest cancers among women. New national guidelines incorporating molecular testing of HPV DNA promise to be a game-changer in prevention, but challenges still remain.
A new era for HPV prevention
Family and community physician Warley Aguiar Simões explains that in recent years a silent revolution has occurred, not in the newspapers, but in the lives of millions of people: vaccination against the human papillomavirus, HPV. Since the SUS integrated the vaccine in 2014, the country has become part of the global vanguard of preventive medicine.
Today, thanks to recent advances and the expansion of national protocols, what seemed like a distant dream – making cervical cancer a rare disease – is beginning to emerge as a concrete possibility.
But are we already close to this goal? To answer, we must examine the five main reasons that make the HPV vaccine one of the most powerful tools in contemporary public health.
1. Prevent cervical cancer: nip it in the bud
The big difference with HPV vaccination is that it addresses the cause, not just the effect. In more than 95% of cases of cervical cancer, the virus is the causative agent. In countries like the UK and Sweden, where vaccination coverage is high, reductions of up to 90% in precancerous lesions and 83% in cervical cancer cases have already been observed in women vaccinated before adolescence.
Brazil also took a decisive step in July 2025, with the publication of the new Brazilian guidelines for cervical cancer screening, approved by SAES/SECTICS Joint Order No. 13. The document formalizes the DNA-HPV molecular test as the main screening method, capable of identifying the virus even before it causes cellular changes. This integration between vaccination and early detection constitutes the central pillar of the global strategy aimed at eliminating the disease.

2. Reduce the risk of other cancers: a beneficial domino effect
HPV is not limited to the cervix. It is associated with tumors of the vulva, vagina, penis, anus and oropharynx in both women and men. Therefore, extending vaccination to boys and girls increases protection and reduces the circulation of the virus in the community.
International research shows that vaccinated men also have a lower risk of developing HPV-related cancers. Vaccination is therefore an act of health equity, a way of protecting everyone, without distinction.
Read the full report in Saúde em Dia, partner of Metropolises.
Follow the Health and Science editor on Instagram and stay up to date with everything on the subject!