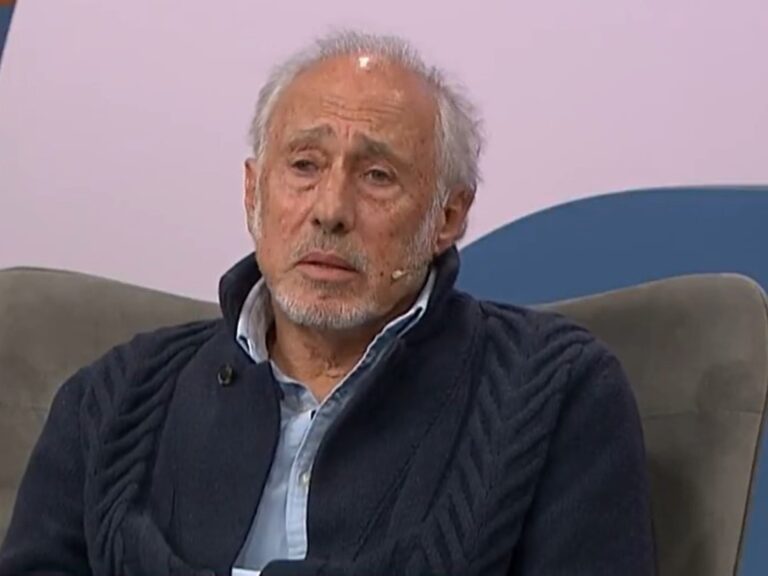
After Tania Saiz suffered a stroke at the age of 47, she began searching for answers. He was not aware of any significant health problems before the episode and had no known family history of cardiovascular disease. But while searching for possible explanations, he discovered a clue to his past.
During her daughter’s pregnancy nearly 20 years earlier, she developed preeclampsia, a complication in which the mother’s blood pressure rises to dangerous levels. She was surprised to discover that the condition had increased her long-term risk of stroke. At the time, doctors did not mention that this problem could influence his health later in life.
For most of modern medicine, the healthcare system has treated pregnancy as a limited event – a nine-month period in a woman’s medical history. Once a woman reaches the end of her pregnancy, the prevailing wisdom is that she more or less returns to her pre-pregnancy state.
But in recent years, more and more evidence has shown that this is not always the case. Experts now believe that pregnancy can provide a window into a woman’s future health and provide valuable information about her long-term risk of heart disease, diabetes, stroke and other cardiovascular diseases.
“What happens during pregnancy doesn’t just end when the baby is born,” says Saiz, now 52 and volunteers as a patient educator for the American Heart Association. If she had known sooner, she said, she could have taken steps to protect herself.
Despite efforts by some medical organizations to raise awareness about these risk factors, few health care providers ask women more than a few months pregnant if they have had complications or manage their care accordingly, experts say.
Failing to screen women with a history of complications is a “missed opportunity” to prevent the disease, says Amy Yu, a stroke neurologist at Sunnybrook Health Sciences Center in Toronto, Canada.
The link between several common pregnancy complications and cardiovascular or metabolic health later in life is important, experts say.
According to leading studies, women who experience hypertensive disorders during pregnancy, which include preeclampsia and high blood pressure and affect approximately 15% of pregnancies in the United States, are at increased risk of almost all cardiovascular health problems, including chronic hypertension, coronary heart disease, heart failure and stroke.
A Mayo Clinic study published last year suggests they also develop coronary heart disease an average of seven years earlier than women without a history. And they are twice as likely to suffer a heart attack that is not caused by a blockage in their main arteries.
The risks are “staggering,” says Vesna Garovic, study co-author and chief of nephrology and hypertension at the Mayo Clinic.
Women diagnosed with gestational diabetes, which affects up to 10% of pregnancies in the United States, are approximately 10 times more likely to be diagnosed with type 2 diabetes compared to women without a history, which itself is linked to heart disease, stroke and dementia.
Gestational diabetes “is really a red flag” for developing diabetes later in life, says Sarah Lassey, co-director of the gestational diabetes program at Brigham and Women’s Hospital, reporting that “your body has some underlying insulin resistance — even if you’ve never had it before, even if you don’t have a family history of diabetes.”
Researchers are still trying to determine whether pregnancy complications lead to various cardiovascular and metabolic problems later in life, or whether they simply reveal a predisposition. Some think it’s a combination of the two.
For now, many experts view pregnancy complications as part of a constellation of risk factors that women should consider when managing their cardiac and metabolic health, as well as their lifestyle and family history.
Lack of awareness
Nearly 15 years ago, the American Heart Association and the American College of Cardiology updated their guidelines to include pregnancy complications as an official risk factor for disease, as evidence of a link began to emerge.
However, new discoveries take a long time to enter medical school curricula and clinical practice (for clinical practice, about 17 years), and many doctors and health professionals are unaware of the risks, says Gina Lundberg, clinical director of Emory’s Women’s Heart Center.
The lack of knowledge among clinicians extends to patients. “It’s not something our mothers and grandmothers knew about,” says Lauren Hassen, director of the Cardiology Postpartum Transition Clinic at The Ohio State University Wexner Medical Center.
Until the end of the 20th century, the medical community believed that heart disease almost exclusively affected men. As a result, the causes of the disease in women are not yet fully understood.
“More women die from heart disease than anything else, and we don’t know all the risk factors,” says Lundberg.
But even with growing evidence of a link between pregnancy and heart disease, standard medical forms don’t typically ask women about pregnancy complications, and patients’ pregnancy records typically don’t follow them through the medical system, so their pregnancy history is often overlooked.
“In these cases, we don’t really have a seamless transition between obstetric care and internal medicine,” Garovic says.
Some experts say more obstetricians are counseling women who have just given birth about long-term risks. But they often struggle with knowing when and how to discuss the lasting implications of what their patients have experienced, especially when their patients have just survived a traumatic pregnancy or childbirth.
“If they give you this information in the heat of the moment, you’re already overwhelmed and terrified for your baby, right? So they often wait for a later appointment, which sometimes never happens,” says Lundberg.
This is why many women ignore the risks. A recent study led by Yu found that fewer than half of women who experienced a cardiovascular or metabolic complication during pregnancy had basic blood pressure, cholesterol, or blood sugar control in the three years after pregnancy.
How to manage your risk
If your primary care doctor doesn’t ask about your pregnancy history, be proactive in mentioning any complications you’ve experienced, recommends Eleni Tsigas, CEO of the Preeclampsia Foundation, a nonprofit advocacy group.
“We don’t need to wait to be diagnosed with diabetes, high blood pressure or heart failure. There are things we can do to stay ahead of the curve.”
Depending on your medical history and pregnancy, a clinician may recommend more frequent or comprehensive screenings for diabetes or heart disease, including more regular measurements of blood pressure, cholesterol, and blood sugar.
Experts also recommend taking basic steps for heart and metabolic health, including a heart-healthy diet, the amount of weekly physical activity recommended by the American Heart Association, and stress and sleep management.
“Most women put themselves last” when it comes to taking care of their own health, Lundberg says. “We kind of lose control of ourselves,” especially when it comes to caring for families, Hassen adds. She and other experts said they hope educating women about these risks will motivate them to take time for themselves.
Saiz, the stroke survivor turned advocate, says she wishes she had the opportunity. “It was never offered to me,” she says. “I think that’s where the real shame comes from.”
This article was originally published in the New York Times.