-
- author, James Gallagher
- To roll, Health and science correspondent for BBC News
A therapy that once seemed like science fiction has helped reverse aggressive, incurable blood cancers in some patients, doctors say.
The treatment involves precisely editing the DNA of white blood cells to transform them into a “living drug” capable of fighting cancer.
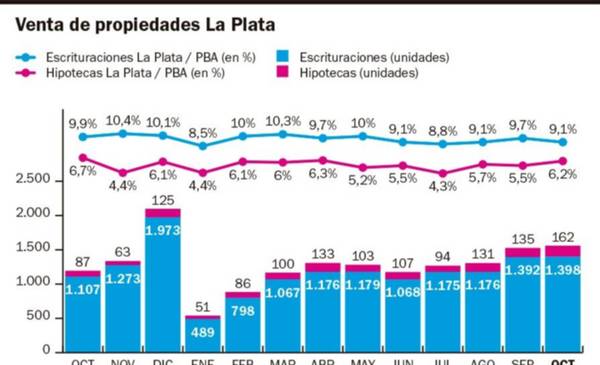
So far, eight other children and two adults with T-cell acute lymphoblastic leukemia have received treatment, and nearly two-thirds (64%) of patients are in remission (this means there are no signs of cancer after treatment, but it doesn’t mean it won’t come back).
T cells function as the body’s defenders – they seek out and eliminate threats – but in this form of leukemia their growth is uncontrollable.
For study participants, chemotherapy and bone marrow transplants did not work. In addition to experimental medicine, all that remained was to provide more comfort at the end of life.
“I really thought I was going to die and I wouldn’t have the chance to grow up and do everything a child deserves to do,” says Alyssa Tapley, 16, from Leicester, UK.
She was the first person in the world to receive treatment at Great Ormond Street Hospital in London and now leads a normal life.

The revolutionary procedure three years ago involved eliminating his old immune system and building a new one. For four months in hospital, she was not able to see her brother, so as not to run the risk of infection.
Today, Alyssa’s cancer is undetectable and she only requires annual screening tests. She is taking her A-levels (UK high school leaving exams), taking part in the Duke of Edinburgh Award (youth development programme), planning driving lessons and planning her future.
“I’m thinking of doing an internship in biomedical sciences and hopefully one day working on blood cancer research as well,” she says.
The team from University College London (UCL) and Great Ormond Street Hospital are using technology called basic edition (edition of the bases, in free translation).
The basics are the language of life. The four types – adenine (A), cytosine (C), guanine (G) and thymine (T) – make up the building blocks of our genetic code. Just as the letters of the alphabet make up meaningful words, the billions of bases in DNA write the instruction manual for the human body.
“Base editing” allows scientists to go to a specific point in the genetic code and change the molecular structure of a single base, converting it to another type and rewriting this manual.
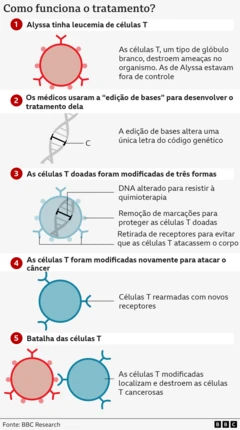
The researchers’ goal was to use the natural ability of healthy T cells, naturally programmed to locate and destroy threats, and target them against T-cell acute lymphoblastic leukemia.
It’s a complex challenge. They had to modify healthy T cells so that they identified diseased cells without the treatment destroying them.
“Dismantle” the immune system
They started with healthy T cells from a donor and began modifying them.
The first basic modification disabled the T cell targeting mechanism, preventing them from attacking the patient’s body.
The second removed the chemical marker CD7, present on all T cells, a crucial step in preventing the therapy from self-destructing.
The third edition created an “invisibility cloak”, preventing cells from being destroyed by a chemotherapy drug.
In the final step, the T cells were instructed to attack any cell carrying the CD7 marker.
So the modified cells would destroy any other T cells they encountered – cancerous or not – but would not attack each other.
The treatment is given by infusion and, if the cancer is not detected after four weeks, the patient receives a bone marrow transplant to rebuild the immune system.
“Even a few years ago this would have been science fiction,” says Professor Waseem Qasim of UCL and Great Ormond Street.
“We need to dismantle virtually the entire immune system,” says Qasim. “It’s an intense treatment, very hard on the patients, but when it works, it works very well.”
The study, published in the scientific journal New England Journal of Medicine (United States), presents the results of the first 11 patients treated at Great Ormond Street and King’s College Hospital (United Kingdom). And it shows that nine of them achieved deep remission, allowing them to undergo a bone marrow transplant.
Seven remain disease-free between three months and three years after treatment.
One of the biggest risks of treatment is infections because the immune system is suppressed.
In two cases, the cancer lost its CD7 markings, allowing it to hide from treatment and reappear in the body.
“Given how aggressive this particular form of leukemia is, these clinical results are quite impressive and I am obviously very pleased that we have been able to give hope to patients who would otherwise have lost it,” says Robert Chiesa, from the Bone Marrow Transplant Unit at Great Ormond Street Hospital.
Deborah Yallop, consultant haematologist at King’s College Hospital, said: “We have seen impressive results in eliminating leukemias that seemed incurable; this is a very powerful approach. »
Commenting on the research, Tania Dexter, chief medical officer at UK stem cell charity Anthony Nolan, said: “Given these patients had little chance of survival before the study, these results provide hope that treatments like this will continue to progress and become available to more patients. »