The neonatology unit of the University Hospital of Guadalajara, dependent on the Castilla-La Mancha Health Service (Sescam), has incorporated important improvements in care and treatment. take care of newborns. The creation by the regional government of a new unit … of Neonatology in the extension building was an opportunity to launch new actions which were not possible in the old premises.
The new Neonatology incorporates improvements which concern not only the well-being of babies and their parents but also the assistance provided, the organization of work and the techniques and procedures it can offer.
The unit It has 13 positions for newborns compared to the nine of the old Neonatology and offers spacious and bright rooms equipped with modern equipment. Likewise, the nursing staff was increased by 19 percent, from eleven to 14 nurses and from seven to twelve auxiliary nursing technicians.
On the one hand, this allowed us to expand the spaces dedicated to care and to create a functional and visible service which facilitates the continuous monitoring of nursing control. On the other hand, the improvements have allowed nursing staff to work, in coordination with pediatric neonatologists, in the development of new lines of work aimed at improving care and early detection of problems in babies.
Likewise, work is underway on updating neonatal care protocols, incorporating the latest scientific evidence, and on implementing new protocols in collaboration with the Quality and Patient Safety area.
In this sense, protocols have been developed regarding the use of ventilators, CPAP machines for the treatment of apnea, a protocol on pneumothorax, one on the kangaroo method and a document relating to tube feeding when the baby needs it or epicutaneous cannulation guided by ultrasound, among others. Its implementation guarantees the quality of processes, reducing variability, and is of great help when training newly hired professionals.
Participation in a national conference
This work of improvement, updating, revision and implementation of work protocols was announced during the XXX Congress of Neonatology and Perinatal Medicine and the Xth Congress of Perinatal Nurses held in Las Palmas de Gran Canaria. Six nurses presented four posters and a resident of the Unit presented a clinical case. With this, they exposed the experience of the new unit and its procedures, as well as the value provided by the new equipment with which it is equipped.
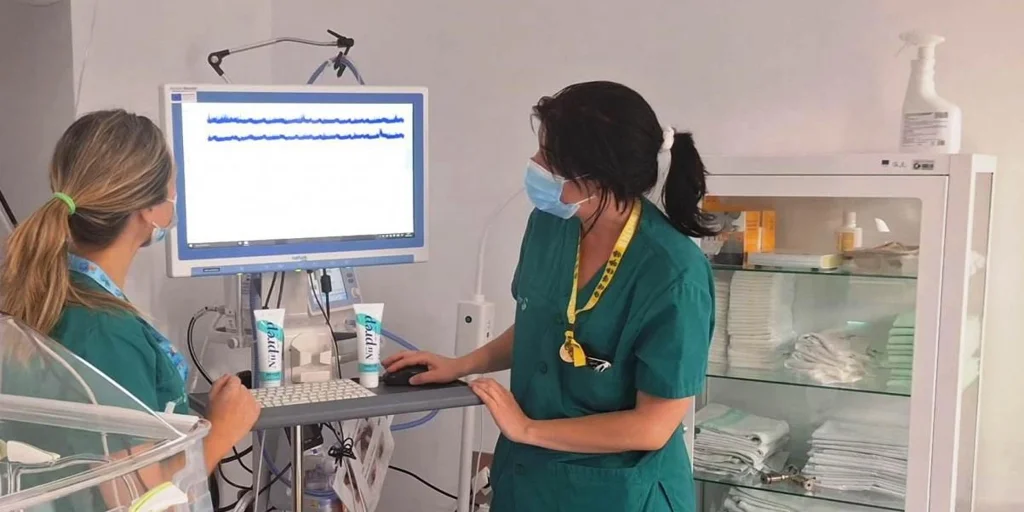
One of the works focused on the new integrated amplitude electroencephalography (EEGA) equipment in neonatal and nursing care, where its usefulness was announced for recognizing seizures in the first moments of life or determining the severity of encephalopathy in a newborn, a problem that can leave long-term consequences and where early detection and action are essential.
The book explained in a simple and visual way how to perform this technique and how to interpret its results. EEGA is generally applied to very premature babies who have movements that suggest seizures, or who have suffered an episode of apnea or who have signs that require checking if there is a neurological problem.
In these cases, and without having to take the baby out of the incubator, electrodes are placed for 24 or 48 hours, during which the baby can be moved and breastfed normally. EEGA measures electrical alterations and allows simple interpretation that facilitates early prognosis and evaluation of neonatal seizures.
Another of the works dealt with the management of neonatal central venous access, raising awareness of the management and care necessary to prevent possible complications.
A third work focused on neonatal necrotizing enterocolitis, a serious inflammatory gastrointestinal disease associated with high morbidity and mortality. The work concluded that this problem occurs particularly in premature newborns with less than 32 weeks of gestation, that feeding with artificial formulas is associated with a higher risk of suffering from it and that nurses play a crucial role in detecting early signs such as abdominal distension, blood in the stools and signs of sepsis, among others.
Finally, they presented the management of bereavement in neonatal intensive care to support families faced with the loss of a newborn. The work delved into the importance of emotional support for families, effective communication for grief management, the role of professionals in promoting the creation of rituals and memories that help in this process, as well as the importance of support and follow-up after loss, providing support and resources from a holistic approach that accompanies and facilitates the onset of grief.



