Leigh syndrome is a rare neurological disease of genetic origin that mainly affects the brain. In many cases, it also affects muscles and other organs. It usually appears in childhood, often in the first years of life, and is linked to failures in energy production within cells. Being a complex pathology, it requires specialized monitoring and constant attention to the evolution of symptoms.
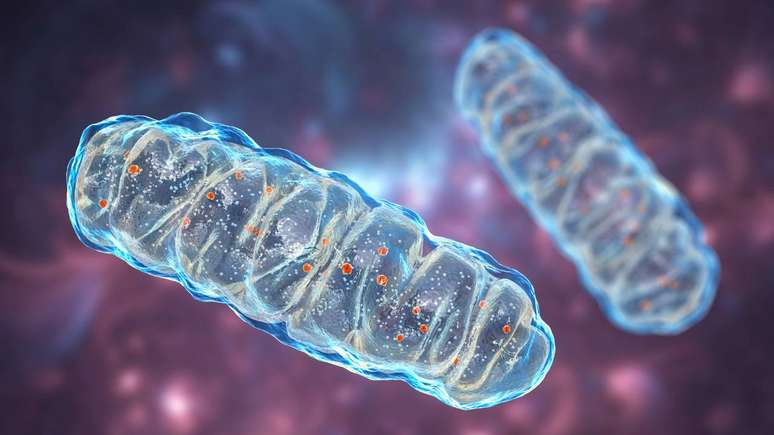
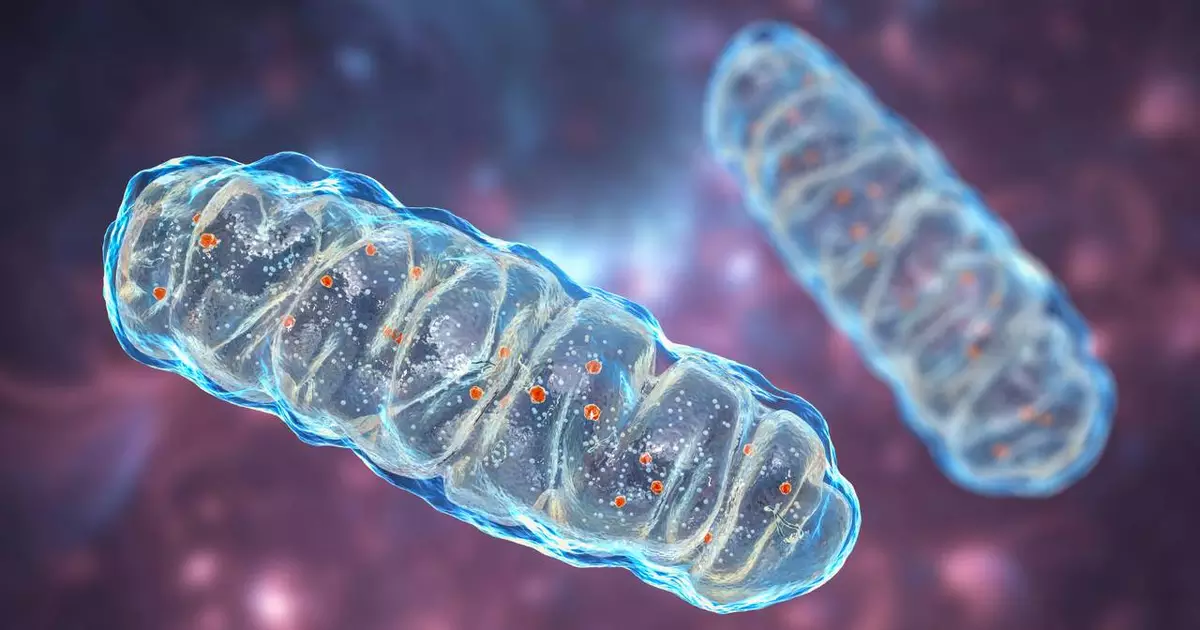
In this syndrome, structures called mitochondria, responsible for producing energy, do not function properly. Thus, this energy failure compromises important areas of the central nervous system. In particular, the brainstem and the basal ganglia. Over time, these regions can undergo degeneration, which explains the appearance of motor, respiratory and cognitive signs at different levels of severity.
What is Leigh syndrome?
Leigh syndrome, also known as subacute necrotizing encephalomyelopathyis a progressive neurodegenerative disease, generally associated with abnormalities of mitochondrial respiration. It can be classified as a mitochondrial disease or as an inborn error of energy metabolism. In addition, although more common in babies and young children, there are reports of cases of appearance in adolescence and adulthood, in forms considered atypical.
From a medical point of view, the syndrome is characterized by symmetrical lesions in certain areas of the brain, visible on imaging tests such as MRI. These injuries are linked to a lack of energy in nerve cells, which eventually no longer resist metabolic stress. The clinical picture is quite variable, but generally involves regression of developmental milestones, muscle weakness, and respiratory changes.
What causes Leigh syndrome?
The main cause of Leigh syndrome is a genetic change that compromises the function of mitochondria, or enzymes involved in energy production. Additionally, these changes can occur in both mitochondrial DNA and nuclear DNA. In addition, depending on the gene affected, the mode of transmission may be different. autosomal recessiveconnected to X chromosome or maternal (when it comes to mitochondrial DNA).
In many cases, Leigh syndrome is linked to defects in mitochondrial respiratory chain complexes, such as complexes I, IV or V, or to a deficiency of pyruvate dehydrogenase. Therefore, this means that the cell cannot convert nutrients into energy efficiently. Among the factors involved are:
- Mutation of mitochondrial genes inherited from the mother;
- Mutation of nuclear genes that control mitochondrial proteins;
- Changes in enzymes essential for energy metabolism;
- Errors in the assembly or maintenance of the respiratory chain.
In some patients, even with advanced genetic testing, the exact causative gene may not be identified immediately, reinforcing the need for detailed investigation and, often, reevaluations over time.
What are the most common symptoms of Leigh syndrome?
Symptoms of Leigh syndrome vary depending on the age of onset, the affected gene, and the degree of nervous system impairment. In general, the first signs appear in childhood, with delays in motor development or a loss of previously acquired skills. Babies who previously held their heads or sat up can no longer perform these activities.
Among the most reported clinical manifestations are:
- Muscle weakness and decreased tone (hypotonia);
- Delay in sitting, crawling or walking;
- Difficulty coordinating movements and instability when moving;
- Changes in breathing, with pauses, irregular or accelerated breathing;
- Swallowing and feeding problems;
- Convulsions or epileptic fits;
- Involuntary eye movements, strabismus or partial loss of vision;
- Growth retardation and short stature in some cases.
In more advanced stages, Leigh syndrome can affect the control of body temperature, blood pressure, and automatic body functions. Some patients experience episodes of sudden worsening following infections, fever, or metabolic stress, requiring special attention in seemingly simple conditions, such as the common cold.
How is Leigh syndrome diagnosed?
The diagnosis of Leigh syndrome is clinical and biological. It begins with observing neurological symptoms and family history, followed by tests evaluating the brain, metabolism and genetic material. Professionals in neurology, medical genetics and other specialties often work together.
Among the most used tests to investigate Leigh syndrome, the following stand out:
- MRI of the brain, which may present typical lesions in deep areas of the brain;
- Dosage of lactic acid in blood and CSF, often at high levels;
- Studies of mitochondrial function in muscle or fibroblasts, when indicated;
- Genetic tests, such as gene panels, exome or genome, to identify the mutation.
Early diagnosis allows for more appropriate surveillance planning, genetic guidance for the family and, when possible, the implementation of therapeutic measures that can slow the progression of the disease.
Is Leigh syndrome treatable?
Until 2025, there is no cure for Leigh syndrome, but there are treatment strategies aimed at relieving symptoms, reducing complications, and attempting to improve quality of life. The care is multidisciplinary and includes neurologists, geneticists, physiotherapists, speech therapists, nutritionists and other professionals.
The most common approaches include:
- Vitamin and cofactor supplementation (such as thiamine, riboflavin, coenzyme Q10, L-carnitine), when tests indicate it;
- Specific diets in certain subtypes, such as carbohydrate restriction in cases of pyruvate dehydrogenase deficiencies;
- Physiotherapy motor and respiratory function to preserve functions and prevent contractures;
- Speech therapy to work on swallowing and communication;
- Nutritional support, with adaptation of food consistency or use of probes, if necessary;
- Seizure control with appropriate antiepileptic drugs;
- Respiratory monitoring and, in some cases, ventilatory assistance.
Ongoing studies are evaluating gene therapies and novel metabolic approaches for mitochondrial diseases, including Leigh syndrome. Although still in the research phase, these strategies broaden the perspective of future options. At the same time, the emphasis remains on continuous monitoring, prevention of metabolic decompensation and comprehensive support of the patient and their family.