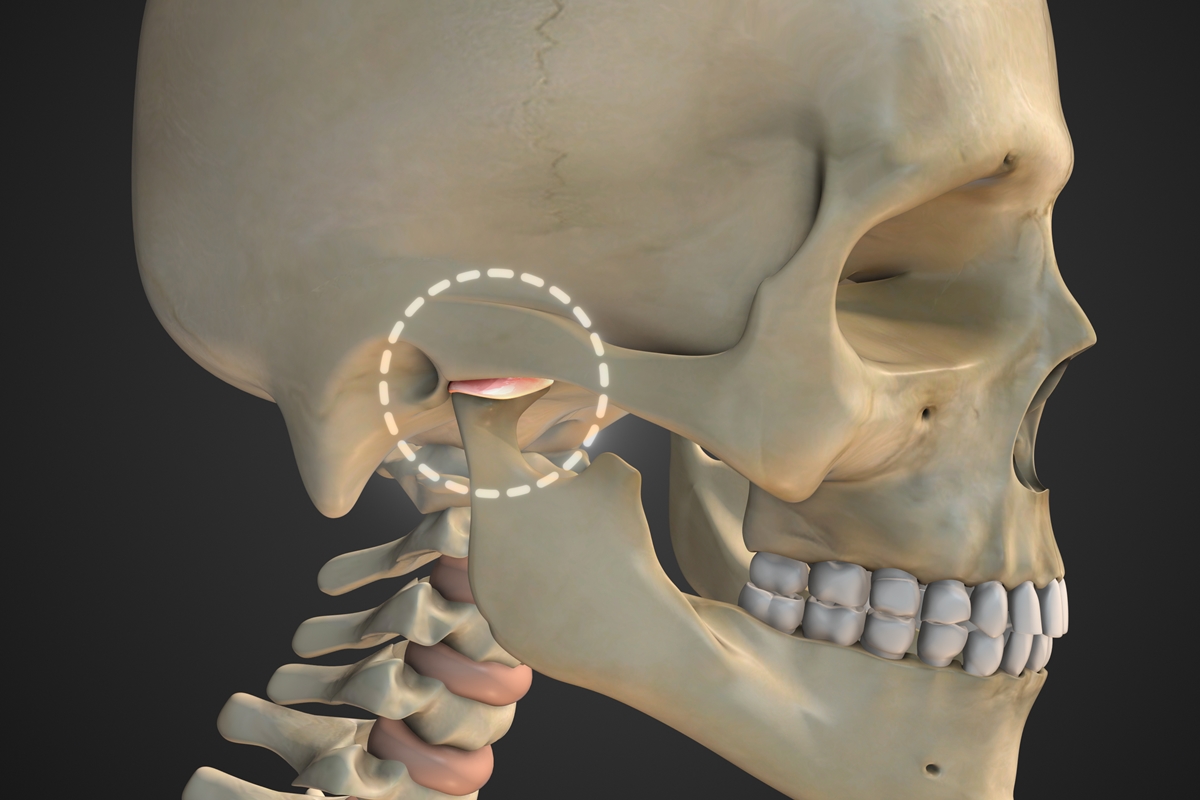
Temporomandibular joint (TMJ) dysfunction is more common than it seems and can present itself in unexpected ways, including persistent ringing in the ears. The TMJ is the joint that connects the jaw to the skull and is involved in essential movements, such as chewing, speaking and yawning.
When it doesn’t work well, muscles and nearby structures become unbalanced, causing pain, joint noises, and in some cases, symptoms that confuse the patient, such as pressure in the ear, facial discomfort, and sound changes.
According to the Ministry of Health, this pathology involves both muscular factors and changes in the joint disc, misalignments and habits that overload the area.
Read also
-
Health
Otorrino teaches how to relieve the pain and sensation of blocked ear
-
Life and style
Nasal washing: the ENT teaches the correct way to clean your nose
-
Health
Covered? Otorrino gives tips for managing ear pain while traveling
-
Special content
Sleep and speech: how going to an ENT can improve your quality of life
Tinnitus, although not the most classic symptom, appears when these changes affect the structures related to the middle and inner ear. This leads many patients to initially consult an otolaryngologist until the origin is identified.
In the office, differentiation begins with audiometry, explains otolaryngologist Jefferson Takehara, from Santa Casa de São José dos Campos.
“Audiometry reveals hearing loss and, in certain cases, can suggest neurological damage, which must be supplemented by specific examinations. When the TMJ is responsible, the test results are generally normal, but the patient’s complaint at the level of the TMJ is important,” believes the doctor.
When to suspect an ATM
Takehara points out that persistent tinnitus without significant auditory or neurological changes raises suspicion of joint dysfunction. The problem is that at first many patients do not notice typical complaints.
“Many experience a feeling of pressure in front of the ear, itching, or a feeling that there is something inside the ear. Some report the feeling of hair inside the ear or tingling, before pain and difficulty chewing develop,” he says.
In case of suspicion, the diagnosis is a diagnosis of exclusion: it is necessary to exclude more frequent and more serious causes before associating tinnitus with TMJ. How the patient describes the sound, factors that aggravate symptoms, and medical history indicate what tests to order and how to conduct the investigation.
It is not recommended to ignore the symptom. “TMJ changes can cause tinnitus, but even tumors such as neuroma can have tinnitus as their first symptom,” Takehara warns. Therefore, any recent, unilateral tinnitus or tinnitus that worsens over time should be evaluated.
Symptoms of TMJ Dysfunction
- Pain or tenderness in the jaw.
- Clicks, noises or blocking when opening the mouth.
- Ear pain without infection.
- Buzzing.
- Frequent headaches.
- Difficulty chewing.
- Pain in the face, neck or shoulders.
- Feeling of pressure in the area near the ear.
Physiotherapy treatment
For physiotherapist Rodrigo Prado, from the Reactive Fisioterapia clinic in Brasilia, the connection between the TMJ and the ear is direct, because the temporomandibular joint shares anatomical and neuromuscular connections with the structures of the ear.
“In cases of dysfunction, mechanical stimuli irritate the trigeminal nerve and modify muscle tension, favoring the appearance of tinnitus and other symptoms,” he explains.
Physiotherapy is generally sufficient when the tinnitus is musculoskeletal, that is to say when it varies during movements of the jaw or neck. In these cases, myofascial release techniques, postural correction and specific exercises reduce pain and stabilize movement.
The structures most involved include the masticatory muscles, upper cervical muscles, and joint components such as the disc and mandibular condyle. Physiotherapeutic evaluation is indicated when tinnitus worsens with chewing, speaking, yawning, clenching teeth, facial pain, clicking, or a history of bruxism.
 Ringing in the ears may be a sign of TMJ dysfunction, a change in the jaw joint that affects facial muscles and structures near the ear.
Ringing in the ears may be a sign of TMJ dysfunction, a change in the jaw joint that affects facial muscles and structures near the ear.
The treatment, Prado reinforces, almost always involves several professionals. In addition to dentists and ENT specialists, speech therapists, psychologists, neurologists, sleep medicine specialists and acupuncture professionals can participate. This integration makes it possible to control emotional, occlusal and postural factors.
There are also habits that make the situation worse. “Bruxism, inadequate posture with the head projected forward, unilateral chewing, frequent chewing gum, biting nails and very hard foods are behaviors that increase tension and overload the TMJ,” reinforces the physiotherapist.
Regarding time to improvement, Prado reports that patients typically notice relief between three and eight weeks, depending on severity and adherence to guidelines. Chronic illnesses progress more slowly, but improvement is usually significant.
Although physiotherapy helps a lot, it is not always enough when done alone. “Even more important is the evaluation of a dental surgeon, to identify situations that lead to joint dysfunction, such as chewing problems, missing or worn teeth, or bruxism,” says Takehara.
During the first consultation, Takehara always recommends examining all possible sources of tinnitus and observing the symptoms associated with chewing and the area in front of the ear.
TMJ dysfunction is a multifactorial problem that can radiate its effects to regions poorly associated with chewing, such as the ears. Recognizing early signs, differentiating the causes of pain, pressure or tinnitus and seeking appropriate evaluation avoids late diagnoses and reduces the risk of worsening.
Through combined treatment and habit changes, most patients experience steady improvement and, in many cases, return to their lives without pain or discomfort.
Follow the Health and Science editor on Instagram and stay up to date with everything on the subject!



